It looks like you're using an Ad Blocker.
Please white-list or disable AboveTopSecret.com in your ad-blocking tool.
Thank you.
Some features of ATS will be disabled while you continue to use an ad-blocker.
share:
I wanted to recap my other thread where I was trying to gather data on Covid-19 and determine if there was any merit to my original theory of it being
2 or more viruses working together.
To that end the first couple of posts here will just be information from that thread organized in a more coherent format.
What I ended up concluding is that Covid is reallly a Virus Like Particle, (VLP) as created by and seen in vaccine research. These are artificial and entirely engineered viral particles with man made protective membranes that are modeled after real viruses.
They are usually cultured and produced in bacteria and only ever have non replicating RNA from viruses so as to provoke immune memory of and defense from said viruses.
I will link the related studies done using VLP, creating coronavirus lipid Membranes, the use of VLP in conjunction with respiratory systems for delivery and general supporting information as it is made available and I digest it.
I wanted to get this organized and coherent but I do welcome contributions so long as we are talking like with like. Alternative theories would probably be better served in their own thread.
The firt study I will discuss replicated a similar virus that they tweaked by adding components of other viruses they knew how to treat already so as to try different methods of treatment should such a reemergence occur.
Most treatments failed and so they warned about the danger such a reemergence of these types of viruses pose.
One part that caught my eye was the part where they went over prior recent epidemics and studied the lineages of those viruses that spread to human and animal populations after crossing over from bats.
The consensus originally thought that Palm Civets (monkey ferret thing) was the species that the SARS virus used to make the spiked Ace2 receptor adaptation after crossover from bats and then to humans. Instead they found that there was direct bat to human transmission and the virus used the Palm Civets as a reservoir type host to supplement the infection of human population clusters.
The infection of both species probably happened simultaneously.The differences weren't very great between the strains that infected either nor were the differences anything more than random. They were of the same lineage. Still they allowed the virus to adapt faster even though its mutation rate was slow and "random".
www.nature.com...
It would be possible that we are seeing such behavior by Covid-19 since there are already confirmed cases of pets and zoo animals testing positive and having gotten it from their owners.
Covid-19 VLP membranes may be limited in their ability to replicate viable copies of themselves since they only have fragments of Viral RNA code inside that are themselves lacking replication associated sequences.
The VLP may just be randomly attaching to cells it can dock with and only having successful replication when the associated code for membrane farming in bacteria is activated.
It also may be infecting our bodies natural bacteria to get a foothold and not even be using our human cells as a primary source of host cells.
That would explain why we arent seeing major genetic changes to the lineages that make their way into other animals /secondary hosts since its not actually adapting to and contending with the new /secondary host immune systems. Its looking for ANY tissue it can hunker down in while in them and tries to replicate.
----------
Oxford university press
Pdf download
-------------
To be continued:
To that end the first couple of posts here will just be information from that thread organized in a more coherent format.
What I ended up concluding is that Covid is reallly a Virus Like Particle, (VLP) as created by and seen in vaccine research. These are artificial and entirely engineered viral particles with man made protective membranes that are modeled after real viruses.
They are usually cultured and produced in bacteria and only ever have non replicating RNA from viruses so as to provoke immune memory of and defense from said viruses.
I will link the related studies done using VLP, creating coronavirus lipid Membranes, the use of VLP in conjunction with respiratory systems for delivery and general supporting information as it is made available and I digest it.
I wanted to get this organized and coherent but I do welcome contributions so long as we are talking like with like. Alternative theories would probably be better served in their own thread.
The firt study I will discuss replicated a similar virus that they tweaked by adding components of other viruses they knew how to treat already so as to try different methods of treatment should such a reemergence occur.
Most treatments failed and so they warned about the danger such a reemergence of these types of viruses pose.
One part that caught my eye was the part where they went over prior recent epidemics and studied the lineages of those viruses that spread to human and animal populations after crossing over from bats.
The consensus originally thought that Palm Civets (monkey ferret thing) was the species that the SARS virus used to make the spiked Ace2 receptor adaptation after crossover from bats and then to humans. Instead they found that there was direct bat to human transmission and the virus used the Palm Civets as a reservoir type host to supplement the infection of human population clusters.
The infection of both species probably happened simultaneously.The differences weren't very great between the strains that infected either nor were the differences anything more than random. They were of the same lineage. Still they allowed the virus to adapt faster even though its mutation rate was slow and "random".
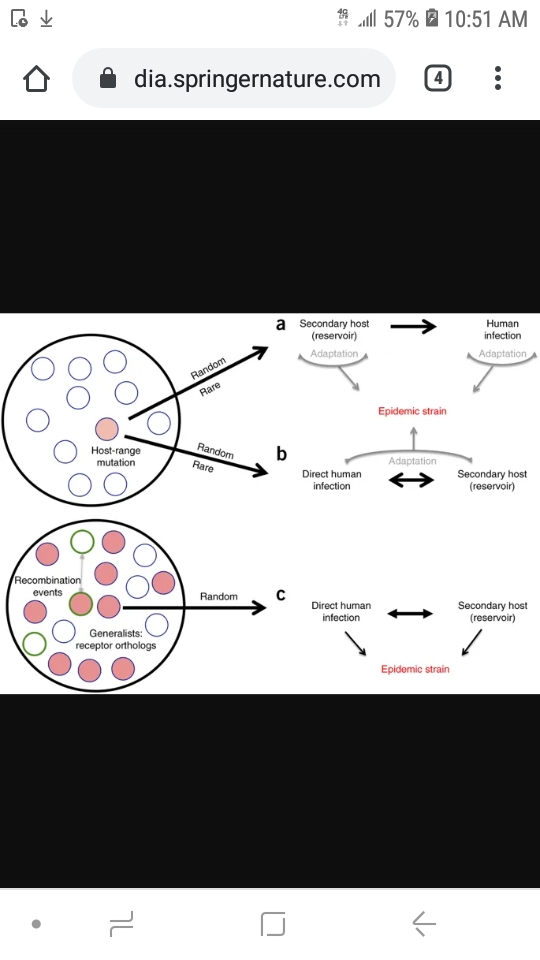
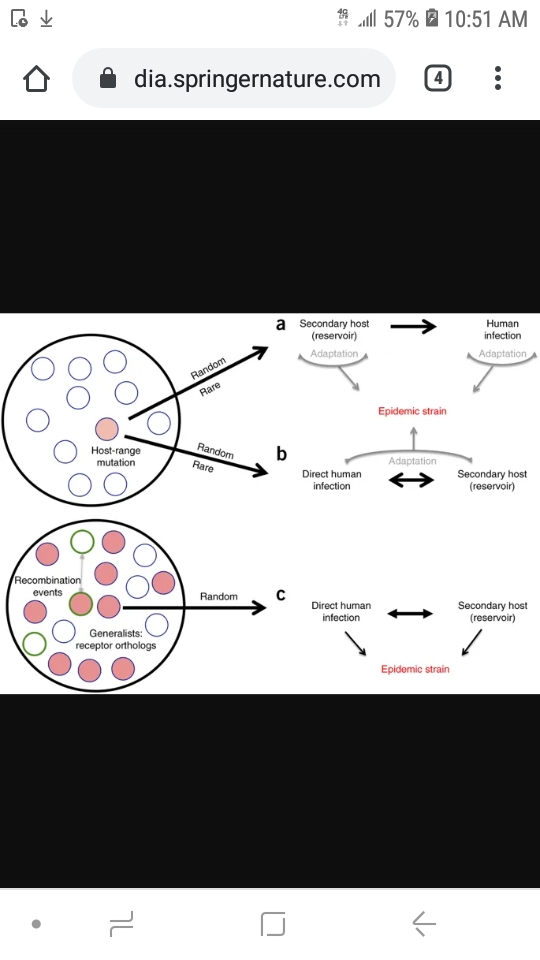
Coronavirus strains are maintained in quasi-species pools circulating in bat populations. (a,b) Traditional SARS-CoV emergence theories posit that host-range mutants (red circle) represent random and rare occurrences that permit infection of alternative hosts.
The secondary-host paradigm (a) argues that a nonhuman host is infected by a bat progenitor virus and, through adaptation, facilitates transmission to humans; subsequent replication in humans leads to the epidemic viral strain.
The direct paradigm (b) suggests that transmission occurs between bats and humans without the requirement of an intermediate host; selection then occurs in the human population with closely related viruses replicating in a secondary host, permitting continued viral persistence and adaptation in both.
(c) The data from chimeric SARS-like viruses argue that the quasi-species pools maintain multiple viruses capable of infecting human cells without the need for mutations (red circles). Although adaptations in secondary or human hosts may be required for epidemic emergence, if SHC014 spike–containing viruses recombined with virulent CoV backbones (circles with green outlines), then epidemic disease may be the result in humans. Existing data support elements of all three paradigms.
www.nature.com...
It would be possible that we are seeing such behavior by Covid-19 since there are already confirmed cases of pets and zoo animals testing positive and having gotten it from their owners.
Covid-19 VLP membranes may be limited in their ability to replicate viable copies of themselves since they only have fragments of Viral RNA code inside that are themselves lacking replication associated sequences.
The VLP may just be randomly attaching to cells it can dock with and only having successful replication when the associated code for membrane farming in bacteria is activated.
It also may be infecting our bodies natural bacteria to get a foothold and not even be using our human cells as a primary source of host cells.
That would explain why we arent seeing major genetic changes to the lineages that make their way into other animals /secondary hosts since its not actually adapting to and contending with the new /secondary host immune systems. Its looking for ANY tissue it can hunker down in while in them and tries to replicate.
----------
RESEARCH ARTICLE
MICROBIOLOGY
On the origin and continuing evolution of SARS-CoV-2
ABSTRACT
The SARS-CoV-2 epidemic started in late December 2019 in Wuhan, China, and has since
impacted a large portion of China and raised major global concern. Herein, we investigated
the extent of molecular divergence between SARS-CoV-2 and other related coronaviruses.
Although we found only 4% variability in genomic nucleotides between SARS-CoV-2 and a bat SARS-related coronavirus (SARSr-CoV; RaTG13), the difference at neutral sites was 17%, suggesting the divergence between the two viruses is much larger than previously estimated.
Our results suggest that the development of new variations in functional sites in the receptor-binding domain (RBD) of the spike seen in SARS-CoV-2 and viruses from pangolin SARSr-CoVs are likely caused by mutations and natural selection besides recombination.
Population genetic analyses of 103 SARS-CoV-2 genomes indicated that these viruses evolved into two major types (designated L and S), that are well defined by two different SNPs that show nearly complete linkage across the viral strains sequenced to date.
Although the L type (~70%) is more prevalent than the S type (~30%), the S type was found to be the ancestral version. Whereas the L type was more prevalent in the early stages of the outbreak in Wuhan, the frequency of the L type decreased after early January 2020.
Human intervention may have placed more severe selective pressure on the L type, which might be
more aggressive and spread more quickly. On the other hand, the S type, which is evolutionarily older and less aggressive, might have increased in relative frequency due to relatively weaker selective pressure.
These findings strongly support an urgent need for
further immediate, comprehensive studies that combine genomic data, epidemiological data,
and chart records of the clinical symptoms of patients with coronavirus disease 2019
(COVID-19).
Keywords: SARS-CoV-2, virus, molecular evolution, population genetics
Oxford university press
Pdf download
-------------
To be continued:
edit on 8-4-2020 by HelloboysImbackguy because: (no reason given)
So what I have learned from your post is that we should eradicate all species of bats from every segment of the Earth.
Here is a study done showing that Rift Valley Fever (RFV) viral proteins were being added to other viruses in VLP form to make chimeric versions for
vaccines. This study shows the effectiveness of making non replicating VLP for vaccines against RVF itself.
www.ncbi.nlm.nih.gov...
What stood out for me:
I wonder if the Wuhan lab was given TSI-GSD-200 and if they can account for all their stock? Was any used for some other research and what was the nature of that research? Universal flu vaccine research? Universal cross species vaccines? Both?
MORPHOLOGY VERY SIMILAR TO THAT OF WILD TYPE!
-------------
Here is evidence that these chimeric VLP were used to develop vaccines and can be introduced via a subjects respiratory systems. This technology has already been developed.
They infected the lungs of chimpanzees with a RVF infused adenovirus. Lets not forget that the RVF virus was already capable of infecting humans and our domesticated animals interchangeably exactly as we see with Covid and SARS.
www.weforum.org...
Was Covid-19 a product of stolen universal vaccine research using the SARS virus as a backbone, that is, a VLP modeled after the coronavirus with these RVF proteins in the RNA, and the ACE2 receptor spike protein engineered into a self replicating membrane, and was it an effort to create a universal Flu vaccine?
One that can be modified effectively to be used against other viruses that affect livestock as well? One that is delivered via airborne viral particles into the respiratory system...
Does covid-19 contain any of these partial RVF viral proteins in its RNA? Does it have any other related genetic fragments that are registered for vaccines?
If we use the same methods in testing that veterinarians use to determine if an animal has a vaccine or an actual replicating virus in its blood, would we see other indicators of covid patients being vaccinated against known viruses?
That too would prove or disprove if Covid is a VLP with related vaccine RNA in its genetic make up and so would HAVE to be vaccine related research since only a lab made vaccine could produce such results.
Added:
Link to the technique this vaccine development used:
www.sciencedirect.com...
A replication-incompetent Rift Valley fever vaccine: Chimeric virus-like particles protect mice and rats against lethal challenge
Robert B. Mandell, Ramesh Koukuntla, [...], and Ramon Flick
Abstract
Virus-like particles (VLPs) present viral antigens in a native conformation and are effectively recognized by the immune system and therefore are considered as suitable and safe vaccine candidates against many viral diseases.
Here we demonstrate that chimeric VLPs containing Rift Valley fever virus (RVFV) glycoproteins GN and GC, nucleoprotein N and the gag protein of Moloney murine leukemia virus represent an effective vaccine candidate against Rift Valley fever, a deadly disease in humans and livestock.
RVFV is a member of the Bunyaviridae family, which includes more than 300 viruses grouped into five genera
(Orthobunyavirus, Hantavirus, Nairovirus, Phlebovirus, and Tospovirus).
Bunyaviruses are enveloped viruses with a tripartite, single-stranded RNA genome of negative and sometimes ambisense polarity
(Elliott, 1996, Elliott et al., 1991, Schmaljohn and Hooper, 2001).
These promising attempts to generate VLP-based vaccines against many different animal and human pathogens encouraged us to evaluate RVF VLPs as vaccine candidates against RVFV. Here we describe the generation of chimeric RVF VLPs, a novel concept for bunyaviruses, the optimization of VLP production and their successful use as vaccine candidates
RVFV is a prototype of emerging/re-emerging pathogens and is classified as a Category A High Priority Pathogen by the National Institute for Allergy and Infectious Diseases (NIAID)
link from study
, is on the Center for Disease Control (CDC) Bioterrorism Agents
link from study
and is also classified as a Department of Health and Human Services (HHS), United States Department of Agriculture (USDA) overlap select agent (USDA, 2005).
www.ncbi.nlm.nih.gov...
What stood out for me:
A formalin-inactivated RVFV vaccine, TSI-GSD-200, has been developed; however, it is not licensed and not commercially available (Pittman et al., 1999). TSI-GSD-200 is only provided to veterinarians working in endemic areas, high containment laboratory workers and others at high risk for contracting RVFV (Pittman et al., 1999). Unfortunately, th
I wonder if the Wuhan lab was given TSI-GSD-200 and if they can account for all their stock? Was any used for some other research and what was the nature of that research? Universal flu vaccine research? Universal cross species vaccines? Both?
Unfortunately, this vaccine is (i) expensive, (ii) difficult to produce, (iii) in short supply, (iv) requires larger dose relative to an attenuated vaccine and three initial inoculations followed by a 6-month booster (v) and requires continued annual boosters to maintain protective immunity (Frank-Peterside, 2000, Kark et al., 1982, Kark et al., 1985, Niklasson et al., 1985).
The use of virus-like particles (VLPs) is a promising approach for the development of a safe and efficient RVFV vaccine.
Expression of structural proteins of many non-enveloped and enveloped viruses leads to the formation of VLPs (Garcea and Gissmann, 2004, Grgacic and Anderson, 2006a, Grgacic and Anderson, 2006b, Noad and Roy, 2003).
Such VLPs frequently exhibit a morphology very similar to that of wild-type (wt) viruses (Johnson and Chiu, 2000).
MORPHOLOGY VERY SIMILAR TO THAT OF WILD TYPE!
-------------
Here is evidence that these chimeric VLP were used to develop vaccines and can be introduced via a subjects respiratory systems. This technology has already been developed.
They infected the lungs of chimpanzees with a RVF infused adenovirus. Lets not forget that the RVF virus was already capable of infecting humans and our domesticated animals interchangeably exactly as we see with Covid and SARS.
Developing the vaccine
Since clinical trials are always the final stage in demonstrating that a vaccine is safe to use in humans, my colleagues and I started by using a technique that has extensively been shown to be safe for human vaccination against a host of diseases, including influenza, malaria, and Ebola.
The technique uses a chimpanzee respiratory (adenovirus) virus to expose individuals to just a small part of the Rift Valley Fever virus – enough for the immune system to recognise a future infection, but not enough to cause an infection in itself.
As this incomplete virus is markedly different to the full virus, the technique allows animal health practitioners to accurately test whether an animal is vaccinated, or an infected but symptomless carrier.
This is crucial during outbreaks, as false positives can lead to unnecessary culling of livestock, increased costs, and reduced cooperation of farmers in the fight to control the disease
www.weforum.org...
Was Covid-19 a product of stolen universal vaccine research using the SARS virus as a backbone, that is, a VLP modeled after the coronavirus with these RVF proteins in the RNA, and the ACE2 receptor spike protein engineered into a self replicating membrane, and was it an effort to create a universal Flu vaccine?
One that can be modified effectively to be used against other viruses that affect livestock as well? One that is delivered via airborne viral particles into the respiratory system...
Does covid-19 contain any of these partial RVF viral proteins in its RNA? Does it have any other related genetic fragments that are registered for vaccines?
If we use the same methods in testing that veterinarians use to determine if an animal has a vaccine or an actual replicating virus in its blood, would we see other indicators of covid patients being vaccinated against known viruses?
That too would prove or disprove if Covid is a VLP with related vaccine RNA in its genetic make up and so would HAVE to be vaccine related research since only a lab made vaccine could produce such results.
Added:
Link to the technique this vaccine development used:
Rapid development of vaccines against emerging pathogens: The replication-deficient simian adenovirus platform technology
www.sciencedirect.com...
edit on 8-4-2020 by HelloboysImbackguy because: (no reason given)
Related to: Virus like particles and artificially created coronavirus lipid protective layer that can be programmed to hold Viral RNA
www.ncbi.nlm.nih.gov...
This study shows that the ability to make a VLP with a coronavirus membrane is possible and already used in vaccine research /treatment.
In this study they essentially built a dummy " shell " coronavirus particle and programmed its self replication...so it could make more shells....which COULD be filled with the genetic fragments of Viruses you want to vaccinate against in a seperate process...
These " Virus Like Particles " are indistinguishable from actual viruses. Their morphology is identical to wild type viruses.
Upon coexpression of M, S, and E by using the vaccinia virus T7 system (20), virus-like particles (VLPs) containing these three viral membrane proteins were assembled in and released from cells.
However, only M and E were required for particle formation. The S protein was dispensable but was incorporated when present (6, 73).
The envelope particles produced by this system were shown to form a homogeneous population of spherical particles indistinguishable from authentic virions in size and shape (73).
One of our main interests is to understand the process of coronavirus assembly.
We are particularly interested in the interactions and the mechanisms that drive the formation of the viral particles. With the VLP assembly system, we have developed an ideal tool for the study of coronavirus envelope formation and for the analysis of the interactions between the viral membrane proteins in molecular detail
www.ncbi.nlm.nih.gov...
This study shows that the ability to make a VLP with a coronavirus membrane is possible and already used in vaccine research /treatment.
In this study they essentially built a dummy " shell " coronavirus particle and programmed its self replication...so it could make more shells....which COULD be filled with the genetic fragments of Viruses you want to vaccinate against in a seperate process...
These " Virus Like Particles " are indistinguishable from actual viruses. Their morphology is identical to wild type viruses.
If they can code DNA or something simple like specific DNA Viral traits into simple RNA virus particles then its a working virus like the real thing
once it can replicate.
Especially if those vaccines and related chimeric viruses become untreatable in lab testing and are not destroyed in the lab...and get out. Then we see exactly this scenario play out.
We see in our case an original strain morphed in a few months into 8 different strains...with 2 types and more to come..
on a slowly mutating timeframe that doesn't account for jumps in natural adaptability...the more agressive and lethal strain, the L type is MORE prevalent 70% than the S type 30% which is the ancestral strain.
Thats backwards. The more agressive ones should die off first or eventually. The softer the virus on the host, the more time it spends spreading.
This is not following rules of natural selection which to me indicates prior reinforcement with normally lost traits, that were purposefully made to go against nature and the possible SLOW mutation into a lethal AND highly contagious strain.
One where these sequences of genetic material become more stable and less prone to mutations and possible genetic deactivation. (Through generational lab enrichment which would coincidentally look like the 3 avenues its evolution took.)
Again, With no evidence of it in the wild to adequately explain its incremental evolution that its genetic evidence suggests.
The evidence does show that Natural selection, recombination, and mutation played a part in its evolution. That would leave TONS of evidence in the wild in other species or human populations. Nothing is there to explain that.
Especially if those vaccines and related chimeric viruses become untreatable in lab testing and are not destroyed in the lab...and get out. Then we see exactly this scenario play out.
We see in our case an original strain morphed in a few months into 8 different strains...with 2 types and more to come..
on a slowly mutating timeframe that doesn't account for jumps in natural adaptability...the more agressive and lethal strain, the L type is MORE prevalent 70% than the S type 30% which is the ancestral strain.
Thats backwards. The more agressive ones should die off first or eventually. The softer the virus on the host, the more time it spends spreading.
This is not following rules of natural selection which to me indicates prior reinforcement with normally lost traits, that were purposefully made to go against nature and the possible SLOW mutation into a lethal AND highly contagious strain.
One where these sequences of genetic material become more stable and less prone to mutations and possible genetic deactivation. (Through generational lab enrichment which would coincidentally look like the 3 avenues its evolution took.)
Again, With no evidence of it in the wild to adequately explain its incremental evolution that its genetic evidence suggests.
The evidence does show that Natural selection, recombination, and mutation played a part in its evolution. That would leave TONS of evidence in the wild in other species or human populations. Nothing is there to explain that.
The past 48 hours or so have seen a huge revelation: COVID-19 causes prolonged and progressive hypoxia (starving your body of oxygen) by binding to the heme groups in hemoglobin in your red blood cells
. People are simply desaturating (losing o2 in their blood), and that’s what eventually leads to organ failures that kill them, not any form of ARDS or pneumonia. All the damage to the lungs you see in CT scans are from the release of oxidative iron from the hemes, this overwhelms the natural defenses against pulmonary oxidative stress and causes that nice, always-bilateral ground glass opacity in the lungs.
Patients returning for re-hospitalization days or weeks after recovery suffering from apparent delayed post-hypoxic leukoencephalopathy strengthen the notion COVID-19 patients are suffering from hypoxia despite no signs of respiratory ‘tire out’ or fatigue.
They would also have those symptoms if there was a virus provoking a viral meningitis in the brain stem and central nervous system.
IMO it's not just affecting red blood cells but tissue in the Medulla that regulates involuntary respiration and heartbeat.
Its causing an inflammation of the brainstem which is having the rest of the effects we see as symptoms when in fact they are specific to each person infected and are in fact ALL symptoms of a meningitis, and not respiratory failure provoked by damaged lungs.
The virus isnt a RESPIRATORY virus alone. It does work in the blood as was alluded to as well but does so to travel to and infect the brain and central nervous system primarily. The lungs are for propogation and not the main reason for infection
. Through a viral meningitis as well as in the brain directly after prolonged exposure, Encephalitis is provoked which swells the brain as well and compounds all symptoms experienced prior.
Covid 19 is a Neurological virus with associated neurological symptoms.
The respiratory aspect is just the propogation tool of the genetic code which uses SARS viral backbone with the ACE2 receptor proteins and other zoonotic viral RNA (RVF IMO) already included and combined within a coronavirus.
Thats why some people have no respiratory issues but all other symptoms...all though consistently getting the fevers, disorientation and body aches associated with an aseptic meningitis leading into a development of Encephalitis in the brain.
www.atsjournals.org...
The issue with testing that I believe is going on is that this RNA virus is really Chimeric with bits and pieces of fragments of other viruses in
it..including the viral coronavirus family we are testing for...
so we have to adjust to look for fragments of sequences of other viruses registered for use in vaccine research...and not just for complete RNA sequences we see in the EXPECTED "wild" coronavirus.
We will have more accurate tests if we apply the same methods veterinarians use in their tests to see if an animal is infected with a live virus or has a non replicating vaccine in its blood. They need to look for fragments of known viral vaccine sequences and see what matches.
so we have to adjust to look for fragments of sequences of other viruses registered for use in vaccine research...and not just for complete RNA sequences we see in the EXPECTED "wild" coronavirus.
We will have more accurate tests if we apply the same methods veterinarians use in their tests to see if an animal is infected with a live virus or has a non replicating vaccine in its blood. They need to look for fragments of known viral vaccine sequences and see what matches.
They are looking at this like its a traditional or expected wild type RESPIRATORY virus.
Its a Chimeric, lab made, zoonotic, VLP based off the SARS coronavirus which had the ACE2 spike protein already and was combined with Rift valley Fever virus vaccine research . RVF virus is a zoonotic virus. These RVF vaccines and related viruses were originally created for universal vaccine research under the onehealth initiative for the Pirbright institute.
The CCP had that available, but not yet licensed RVF vaccine, that is approved for limited use on various outbreak areas for that disease and MALARIA among others...its only held by vanguard labs due to prohibitive cost and security access concerns.
The CCP was given a stockpile of it for use in China or Africa under agreements with the WHO.
Their thousand talons plan was about POOLING available research from global talent and available knowledge to jump start Chinese EVERYTHING.
Military considerations in terms of biological weapons development were guised under the pretense of defense stragies for China against biological warfare...but certain vaccines are dual agents in their categorization for international disease control guidelines.
Like this RVF vaccine research was considered agricultural since it treated livestock and their associated human populations simultaneously..but could be morphed into useful weapons research. So it was a select dual agent in categorization as well.
Which is what the CCP did. It combined the RVF viral onehealth vaccine research and derived technologies into a Chimeric coronavirus....with possible adenovirus genetic material (simian and human DNA virus family) possibly taken from the clinical trials of RVF zoonotic vaccine research on simians which was done in order to progress and get approval for human trials.
Its a Chimeric, lab made, zoonotic, VLP based off the SARS coronavirus which had the ACE2 spike protein already and was combined with Rift valley Fever virus vaccine research . RVF virus is a zoonotic virus. These RVF vaccines and related viruses were originally created for universal vaccine research under the onehealth initiative for the Pirbright institute.
The CCP had that available, but not yet licensed RVF vaccine, that is approved for limited use on various outbreak areas for that disease and MALARIA among others...its only held by vanguard labs due to prohibitive cost and security access concerns.
The CCP was given a stockpile of it for use in China or Africa under agreements with the WHO.
Their thousand talons plan was about POOLING available research from global talent and available knowledge to jump start Chinese EVERYTHING.
Military considerations in terms of biological weapons development were guised under the pretense of defense stragies for China against biological warfare...but certain vaccines are dual agents in their categorization for international disease control guidelines.
Like this RVF vaccine research was considered agricultural since it treated livestock and their associated human populations simultaneously..but could be morphed into useful weapons research. So it was a select dual agent in categorization as well.
Which is what the CCP did. It combined the RVF viral onehealth vaccine research and derived technologies into a Chimeric coronavirus....with possible adenovirus genetic material (simian and human DNA virus family) possibly taken from the clinical trials of RVF zoonotic vaccine research on simians which was done in order to progress and get approval for human trials.
Its a delivery system of Viral particles via aerosols used in vaccines modeled after a SARS type coronavirus for its natural and mapped qualities.
www.ncbi.nlm.nih.gov...
Morphology Similar to wildtype...check
Is a vaccine that mimics a viruses structure but is a viral particle...check
Carries some genetic material of a Virus, or multiple viruses,...check
Is RNA based with possible viral DNA....check
It isnt a complete SINGLE virus but is MULTIPLE viruses at once...check
...and is delivered via respiratory systems...check...
so any virus that does that besides the already used adenoviruses would be a probable candidate for new vaccine research.
Especially a SARS strain with ACE2 proteins and the ability to infect humans and animals interchangeably...which was the zoonotic quality both RVF and the SARS virus shared and the shared quality that made combining them make sense from a research standpoint.
Especially since RVF viruses already had a semi working vaccine family and mature related technologies already developed and available to the CCP.
Especially if you are piggybacking on onehealth universal vaccine research and you, the CCP, want to produce the first universal flu vaccine with dual use in humans and livestock/ animals and against known and emerging viral threats...
The coronavirus structure is also good since it can store ALOT OF RNA. It has lots of unused potential for adding in more of something else like vaccines do regularly to provoke an immune alertness to the actual viruses and is built already to the task I argue the CCP researchers saw as well.
A formalin-inactivated RVFV vaccine, TSI-GSD-200, has been developed; however, it is not licensed and not commercially available (Pittman et al., 1999). TSI-GSD-200 is only provided to veterinarians working in endemic areas, high containment laboratory workers and others at high risk for contracting RVFV (Pittman et al., 1999). Unfortunately, th
Unfortunately, this vaccine is (i) expensive, (ii) difficult to produce, (iii) in short supply, (iv) requires larger dose relative to an attenuated vaccine and three initial inoculations followed by a 6-month booster (v) and requires continued annual boosters to maintain protective immunity (Frank-Peterside, 2000, Kark et al., 1982, Kark et al., 1985, Niklasson et al., 1985).
The use of virus-like particles (VLPs) is a promising approach for the development of a safe and efficient RVFV vaccine.
Expression of structural proteins of many non-enveloped and enveloped viruses leads to the formation of VLPs (Garcea and Gissmann, 2004, Grgacic and Anderson, 2006a, Grgacic and Anderson, 2006b, Noad and Roy, 2003).
Such VLPs frequently exhibit a morphology very similar to that of wild-type (wt) viruses (Johnson and Chiu, 2000).
www.ncbi.nlm.nih.gov...
Morphology Similar to wildtype...check
Is a vaccine that mimics a viruses structure but is a viral particle...check
Carries some genetic material of a Virus, or multiple viruses,...check
Is RNA based with possible viral DNA....check
It isnt a complete SINGLE virus but is MULTIPLE viruses at once...check
...and is delivered via respiratory systems...check...
so any virus that does that besides the already used adenoviruses would be a probable candidate for new vaccine research.
Especially a SARS strain with ACE2 proteins and the ability to infect humans and animals interchangeably...which was the zoonotic quality both RVF and the SARS virus shared and the shared quality that made combining them make sense from a research standpoint.
Especially since RVF viruses already had a semi working vaccine family and mature related technologies already developed and available to the CCP.
Especially if you are piggybacking on onehealth universal vaccine research and you, the CCP, want to produce the first universal flu vaccine with dual use in humans and livestock/ animals and against known and emerging viral threats...
The coronavirus structure is also good since it can store ALOT OF RNA. It has lots of unused potential for adding in more of something else like vaccines do regularly to provoke an immune alertness to the actual viruses and is built already to the task I argue the CCP researchers saw as well.
Those are most of my thoughts up to now on this subject. I wanted to get them all down along with my supporting evidence and reasoning. Sorry if it
was a boring read but there isnt anything too exciting about this beyond the actual conspiracy surrounding its release. Accidental or intentional. It
IS vaccine research regardless.
Added:
Crash course on vaccines:
Added:
Crash course on vaccines:
edit on 8-4-2020 by HelloboysImbackguy because: (no reason given)
Here is an article about VLP vaccines being developed to treat Covid-19
Well, damn. That was fast.
www.biospace.com...
Medicago Announces Production of a Viable Vaccine Candidate for COVID-19
Published: Mar 12, 2020
The biopharma successfully produced Virus-Like Particles (VLP) of the coronavirus in just 20 days using proprietary plant-based technology
Medicago’s platform can produce both vaccine and antibody candidates against COVID-19 disease
Well, damn. That was fast.
The company uses a proprietary plant-based technology to develop protein-based therapeutics. Unlike traditional vaccination development, Medicago does not use animal products or live viruses to create its products. Instead, it uses Virus-Like Particles (VLPs) that mimic the shape and dimensions of a virus, which allows the body to recognize them and create an immune response in a non-infectious way.
QUEBEC CITY, Quebec--(BUSINESS WIRE)--Medicago, Inc., a biopharmaceutical company headquartered in Quebec City, announced today that they have successfully produced a Virus-Like Particle (VLP) of the coronavirus just 20 days after obtaining the SARS-CoV-2 (virus causing the COVID-19 disease) gene.
Medicago is also using its technology platform to develop antibodies against SARS-CoV-2 in collaboration with the Laval University’s Infectious Disease Research Centre headed by Dr. Gary Kobinger, who helped develop a vaccine and treatment for Ebola. These SARS-CoV-2 antibodies could potentially be used to treat people infected by the virus. This research is being funded, in part, by the Canadian Institutes for Health Research (CIHR).
www.biospace.com...
edit on 8-4-2020 by HelloboysImbackguy because: (no reason given)
Since the evolution of my theory led me to believe that this is vaccine research, I will try to keep track of any viable vaccines against it as the
info is made available.
World Health Organization › ...PDF
DRAFT landscape of COVID-19 candidate vaccines - World Health Organization
World Health Organization › ...PDF
DRAFT landscape of COVID-19 candidate vaccines - World Health Organization
Study on self replicating VLP vaccines
ADDED:
Here is a study using Replicon RNA.
Delivery of self-amplifying RNA vaccines in in vitro reconstituted virus-like particles
Many mRNA-based vaccines have been investigated for their specific potential to activate dendritic cells (DCs), the highly-specialized antigen-presenting cells of the immune system that play a key role in inducing effective CD4+ and CD8+ T-cell responses. In this paper we report a new vaccine/gene delivery platform that demonstrates the benefits of using a self-amplifying (“replicon”) mRNA that is protected in a viral-protein capsid.
ADDED:
Here is a study using Replicon RNA.
In vitro evolution of enhanced RNA replicons for immunotherapy
Scientific Reports volume 9, Article number: 6932 (2019) Cite this article
3619 Accesses
2 Altmetric
Metricsdetails
Abstract
Self-replicating (replicon) RNA is a promising new platform for gene therapy, but applications are still limited by short persistence of expression in most cell types and low levels of transgene expression in vivo.
To address these shortcomings, we developed an in vitro evolution strategy and identified six mutations in nonstructural proteins (nsPs) of Venezuelan equine encephalitis (VEE) replicon that promoted subgenome expression in cells.
edit on 8-4-2020 by HelloboysImbackguy because: (no reason given)
wow, buddy. you are smart! great job!
i read the whole thing and found it fascinating. i think you are spot on about the primary target being the nervous system. i have read about the fact that the biggest reason people stop breathing is because the nervous impulse from the medulla.... just stops working?
BUT, i am not convinced about the VLP/vaccine angle. if it is indistinguishable from the wild type, what is it that, for you, convinces you that the RNA is not a single independently operating molecule?
why MUST it be fragments?
thanks for the great read.
danny.
i read the whole thing and found it fascinating. i think you are spot on about the primary target being the nervous system. i have read about the fact that the biggest reason people stop breathing is because the nervous impulse from the medulla.... just stops working?
BUT, i am not convinced about the VLP/vaccine angle. if it is indistinguishable from the wild type, what is it that, for you, convinces you that the RNA is not a single independently operating molecule?
why MUST it be fragments?
thanks for the great read.
danny.
a reply to: tgidkp
Hey,
I dont think it must ONLY contain fragments. My thinking was more down the line of detection for testing accuracy or for treatment. If it did originally start off as a lab trial vaccine it would probably have registered safe segments of RNA sequencing used in other vaccines.
Vaccines use segments of viral genetic material to make the immune system create a memory for the viruses these fragments were taken from without risking those viruses infecting a host.
I am arguing that either the RNA used was or had Replicon RNA. That or a self replicating lipid structure with imbeded Viron RNA that eirher recombined to be complete or was made so by the process of the membrane's replication code being expressed randomly to in some way alter the RNA it is carrying.
Also I suspect that the initial infection has the VLP infect our natural digestive bacterias (OR OTHERS) and move on from there.
Older people tend to have higher bacteria levels than younger people. They are also more susceptible to neurological issues and the resulting cascading organ failure.
Just a hunch. I am open to it being another form of Vaccine delivery method or other Vaccine type, but I am fairly convinced it is a lab culture that became untreatable and was not properly destroyed.
It being a VLP most fits with the evidence and the available research the CCP would have pooled /hodgepodged with considerations to their global partnerships with the WHO and the access that grants them to select dual use biological agents. Also I am considering the CCPs thousand talons initiative with its rumored achievements.
I also wonder if any DNA sequences from an adenovirus have also been incorporated into the lipid protective layer's mechanism for self replication and harvesting from bacteria.
If that somehow made it possible for the RNA it injects to become a live viron on the other end of replication, complete with all relevant code when the new VLP are produced in bacteria.
Then these few (at first) randomly produced live virus particles infect an appropriate host cell following the expression of some or multiple sections of RNA from whatever real virus or viruses they were originally a vaccine for.
I am open to that aspect evolving or being completely discarded eventually. It just fits the profile.
Adenovirus membranes are exceptionally resistant and make their DNA based viruses very robust.
It would be possible to express that particular set of traits in an RNA based virus if the actual proteins were mapped and understood by the research community, which they seem to be.
Cheers. Glad you liked it!
Have a good one.
Hey,
I dont think it must ONLY contain fragments. My thinking was more down the line of detection for testing accuracy or for treatment. If it did originally start off as a lab trial vaccine it would probably have registered safe segments of RNA sequencing used in other vaccines.
Vaccines use segments of viral genetic material to make the immune system create a memory for the viruses these fragments were taken from without risking those viruses infecting a host.
I am arguing that either the RNA used was or had Replicon RNA. That or a self replicating lipid structure with imbeded Viron RNA that eirher recombined to be complete or was made so by the process of the membrane's replication code being expressed randomly to in some way alter the RNA it is carrying.
Also I suspect that the initial infection has the VLP infect our natural digestive bacterias (OR OTHERS) and move on from there.
Older people tend to have higher bacteria levels than younger people. They are also more susceptible to neurological issues and the resulting cascading organ failure.
Just a hunch. I am open to it being another form of Vaccine delivery method or other Vaccine type, but I am fairly convinced it is a lab culture that became untreatable and was not properly destroyed.
It being a VLP most fits with the evidence and the available research the CCP would have pooled /hodgepodged with considerations to their global partnerships with the WHO and the access that grants them to select dual use biological agents. Also I am considering the CCPs thousand talons initiative with its rumored achievements.
I also wonder if any DNA sequences from an adenovirus have also been incorporated into the lipid protective layer's mechanism for self replication and harvesting from bacteria.
If that somehow made it possible for the RNA it injects to become a live viron on the other end of replication, complete with all relevant code when the new VLP are produced in bacteria.
Then these few (at first) randomly produced live virus particles infect an appropriate host cell following the expression of some or multiple sections of RNA from whatever real virus or viruses they were originally a vaccine for.
I am open to that aspect evolving or being completely discarded eventually. It just fits the profile.
Adenovirus membranes are exceptionally resistant and make their DNA based viruses very robust.
It would be possible to express that particular set of traits in an RNA based virus if the actual proteins were mapped and understood by the research community, which they seem to be.
Cheers. Glad you liked it!
Have a good one.
edit on 8-4-2020 by HelloboysImbackguy because: (no reason given)
originally posted by: HelloboysImbackguy
a reply to: tgidkp
you know, i super enjoy reading you. you have a vivid imagination combined with exceptional research.
=== i think you might just be right.
=== good stuff.
a reply to: tgidkp
.... a self replicating lipid structure with imbeded Viron RNA...
.... harvesting from bacteria....
you know, i super enjoy reading you. you have a vivid imagination combined with exceptional research.
=== i think you might just be right.
=== good stuff.
edit on 2020-04-08T20:26:57-05:0008America/Chicago04C-0500Apr-05:00 by tgidkp because: (no reason given)
Here is a great read concerning testing and how looking for a general history of infection by the presence of Antigens in the blood is more accurate
than actually testing and comparing sampled viral RNA.
Other types of tests amplify sections of viral genetic material taken from samples off swabs and such, and compare their genetic makeup to that of known viruses. That requires complex Equipment and is flawed.
I say its additionally flawed because they only amplify and compare a small portion of genetic material and so wouldn't accurately test for chimeric Viruses that have a hodgepodged genetic makeup.
In the article they advocate for testing methods that test for antibodies against covid being present in the blood. Their level dictates if and when you were infected. If you are inoculated or are getting to that point because you are in fact infected.
I say that Covid patients are also inoculated against something else, and knowing what that other threat(s) their immune systems saw and now remember would prove what vaccine research this came from.
thenativeantigencompany.com...
An interesting note on what is being seen as far as symptoms:
Lets take a Look at the table with listed symptoms and their frequency...
Fever, dry cough, shortness of breath, and diarrhea are the common symptoms.
Head aches, sore throat, aches and pains and fatigue are the less common but still widely seen symptoms.
To me the secondary symptoms are themselves a product of the primary symptoms.
The overlapping issue is the viral load. The study I jlinked is quoted saying that viral load varies in the respiratory tract between infections. That the viral load in the respiratory system is over all very low, even in people with acute respiratory failure.
To me its a matter of reactivated Virus particles producing enough viable replicating particles to saturate the blood until enough can make it out and infect a new host with replicating virus particles.
I think most viral particles produced in the body are duds, but those duds still sometimes attach to cells and interfere with their oxygenation.
The ones that arent duds do inject the host cells with replication capable viral RNA but its not stable so only a small percentage of those replicated Virus particles are themselves viable copies.
The sheer amount produced guarantees that some hosts will produce some viable viral particles and perpetuate the infection in a population.
Also considering the viruses ability to infect animals and use them as reservoir host pools /reinforce the infection, this theory would still be viable and explain what is being seen.
Other types of tests amplify sections of viral genetic material taken from samples off swabs and such, and compare their genetic makeup to that of known viruses. That requires complex Equipment and is flawed.
I say its additionally flawed because they only amplify and compare a small portion of genetic material and so wouldn't accurately test for chimeric Viruses that have a hodgepodged genetic makeup.
In the article they advocate for testing methods that test for antibodies against covid being present in the blood. Their level dictates if and when you were infected. If you are inoculated or are getting to that point because you are in fact infected.
I say that Covid patients are also inoculated against something else, and knowing what that other threat(s) their immune systems saw and now remember would prove what vaccine research this came from.
RT-PCR is the workhorse of viral diagnosis and has been invaluable in COVID-19 case confirmation and isolation guidance.
However, while fast and sensitive, PCR suffers from some inherent drawbacks that limit it to diagnosis during the acute phase of infection.
To better understand the transmission dynamics of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and develop effective countermeasures against it, antigen- and antibody-based immunoassays will be essential.
In this blog, we explain the key differences between PCR and immunoassays for COVID-19 diagnosis, and present our growing pipeline of coronavirus reagents for the development of highly accurate diagnostic kits
However, the biggest advantage of immunoassays is their ability to detect past infections.
Once a patient has recovered from COVID-19 and virus is cleared from the body, viral RNA is no longer available for detection in the respiratory tract, leaving only a short window during the acute stage of infection in which SARS-CoV-2 can be detected.
While this works well for the diagnosis of ongoing infections, it gives no indication of whether a patient has had the infection historically, and what their immune status is (i.e. if they are immune to COVID-19 or still susceptible to infection).
Unlike RNA, antibodies are long-lasting and can persist in the bloodstream for many years after infection. As such, immunoassays enable us to identify patients that have had COVID-19, retrospectively.
The type of antibody and its relative levels could also be used to indicate the stage of infection and estimate time since exposure for contact tracing.
However, antibody tests have their limitations too. As immunological data continues to emerge, it is becoming apparent that the body’s antibody response to COVID-19 is slow – considerably slower than we might expect.
While data at this point is still limited, it appears that the initial IgM antibody response doesn’t peak until ~9 days after initial infection and the IgG antibody response doesn’t peak until day ~11 [8][9].
thenativeantigencompany.com...
An interesting note on what is being seen as far as symptoms:
As a disease, COVID-19 shows considerable symptomatic variation. Individuals may present with no symptoms at all, while some may have a mild cough and fever, and an unlucky few may experience severe pneumonia and respiratory failure [1]. To complicate matters, COVID-19’s most common symptoms strongly overlap with those presented by other co-circulating respiratory illnesses:
Lets take a Look at the table with listed symptoms and their frequency...
Fever, dry cough, shortness of breath, and diarrhea are the common symptoms.
Head aches, sore throat, aches and pains and fatigue are the less common but still widely seen symptoms.
To me the secondary symptoms are themselves a product of the primary symptoms.
The overlapping issue is the viral load. The study I jlinked is quoted saying that viral load varies in the respiratory tract between infections. That the viral load in the respiratory system is over all very low, even in people with acute respiratory failure.
To me its a matter of reactivated Virus particles producing enough viable replicating particles to saturate the blood until enough can make it out and infect a new host with replicating virus particles.
I think most viral particles produced in the body are duds, but those duds still sometimes attach to cells and interfere with their oxygenation.
The ones that arent duds do inject the host cells with replication capable viral RNA but its not stable so only a small percentage of those replicated Virus particles are themselves viable copies.
The sheer amount produced guarantees that some hosts will produce some viable viral particles and perpetuate the infection in a population.
Also considering the viruses ability to infect animals and use them as reservoir host pools /reinforce the infection, this theory would still be viable and explain what is being seen.
edit on 9-4-2020 by HelloboysImbackguy because: (no reason given)
a reply to: HelloboysImbackguy
You know... i see you do all this research and describe the attack vetor of the virus, and go on to describe across ten posts how people are essentially dying from hypoxemia. GM and others want 1 billion dollars to make ventillators -- which sadly are only effective in cases where the lungs cease to function. We do not have such cases, so I am surprised that I do not see anyone, and you in particular in all your research, talking about ECMO being the real solution for critical cases. We know the symptoms. We know the effects on the body. Its time to start focusing on the remedy. If i see one more COVID thread talking about the symptoms im gonna go nuts. Intubation is not effective unless your lungs stopped working on their own. If I was hospitalized for COVID-19 I would demand they monitor my oxygen saturation and put me on ECMO. Looking forward to your thread on the remedies to mitigate the primary diagnosis and put oxygen back into the bloodstream.
You know... i see you do all this research and describe the attack vetor of the virus, and go on to describe across ten posts how people are essentially dying from hypoxemia. GM and others want 1 billion dollars to make ventillators -- which sadly are only effective in cases where the lungs cease to function. We do not have such cases, so I am surprised that I do not see anyone, and you in particular in all your research, talking about ECMO being the real solution for critical cases. We know the symptoms. We know the effects on the body. Its time to start focusing on the remedy. If i see one more COVID thread talking about the symptoms im gonna go nuts. Intubation is not effective unless your lungs stopped working on their own. If I was hospitalized for COVID-19 I would demand they monitor my oxygen saturation and put me on ECMO. Looking forward to your thread on the remedies to mitigate the primary diagnosis and put oxygen back into the bloodstream.
a reply to: drewlander
I didnt want to delve into treatment since I have no medical training and should not recommend a treatment.
That said, I think hyperbaric oxygen therapy or nitric oxide treatments would work nicely. ECMO looks promising.
Hyperbaric chambers are tough to come by but THAT is going to be an instant fix IMO. The west coast uses them in spas and such. They have smaller individual units than those we see divers use.
Problems arise when an entire country cant get the treatment though.
Any oxygen therapy treatment would keep people alive and doing well. There are new ones and Im am not informed enough to pick one I think would be as effective as hyperbaric therapies.
Also, I am still trying to pinpoint what Viruses were used to create this and what relevant genetic material are we contending with.
Another consideration is that this bug may be using our natural bacterias as the real host cells it is infecting and using for replication...and even with effective oxygenation treatment, unless the underlying cause is treated the patients will just come right back to the hospital when their viral count goes back up and suffocates their red blood cells.
I say reduce the swelling from the meningitis. With that out of the way, let the kidneys do their thing.
If you can, get into a hyperbaric chamber.
I didnt want to delve into treatment since I have no medical training and should not recommend a treatment.
That said, I think hyperbaric oxygen therapy or nitric oxide treatments would work nicely. ECMO looks promising.
Hyperbaric chambers are tough to come by but THAT is going to be an instant fix IMO. The west coast uses them in spas and such. They have smaller individual units than those we see divers use.
Problems arise when an entire country cant get the treatment though.
Any oxygen therapy treatment would keep people alive and doing well. There are new ones and Im am not informed enough to pick one I think would be as effective as hyperbaric therapies.
Also, I am still trying to pinpoint what Viruses were used to create this and what relevant genetic material are we contending with.
Another consideration is that this bug may be using our natural bacterias as the real host cells it is infecting and using for replication...and even with effective oxygenation treatment, unless the underlying cause is treated the patients will just come right back to the hospital when their viral count goes back up and suffocates their red blood cells.
I say reduce the swelling from the meningitis. With that out of the way, let the kidneys do their thing.
If you can, get into a hyperbaric chamber.
edit on 9-4-2020 by HelloboysImbackguy because: (no reason given)
I'm just concerned that this could be a ploy to develop a "vaccine" to give to the majority of the worlds population ..
new topics
top topics
-
Federal law trumps state and local law every time
Social Issues and Civil Unrest: 13 hours ago, 16 flags
active topics
-
Federal law trumps state and local law every time
Social Issues and Civil Unrest • 30 • : ADVISOR -
Elon Says It’s ‘Likely’ He Buys Tanking MSNBC
Political Ideology • 81 • : WeMustCare -
I thought Trump was the existential threat?
World War Three • 79 • : visitedbythem -
Well, here we go red lines crossed Biden gives the go ahead to use long range missiles
World War Three • 394 • : Xtrozero -
-@TH3WH17ERABB17- -Q- ---TIME TO SHOW THE WORLD--- -Part- --44--
Dissecting Disinformation • 3381 • : Crazierfox -
Joe Biden Dabs Away Tears at Farewell White House Dinner
Politicians & People • 25 • : RazorV66 -
A Mysterious Orb filmed over NYC by local news
Aliens and UFOs • 26 • : DaydreamerX -
Anyone like the Scorpions?
Music • 21 • : belkide -
Comcast dumping MSNBC
Mainstream News • 36 • : Kaiju666 -
Post A Funny (T&C Friendly) Pic Part IV: The LOL awakens!
General Chit Chat • 7831 • : DBCowboy
